I get asked a lot about hives at the pharmacy level, especially during summer days, maybe because the triggering factors are more during the season, with increased outdoor activities, food, and fun experiences.
The other dilemma I have is time. We don’t usually have that much time to discuss all the information needed for your success to manage hives.
We are talking about simple hives (acute urticaria) that started a day or two ago, not the long-standing type (chronic urticaria) that requires a doctor’s visit. Although it might start as acute and continue to reappear for more than 6 weeks that’s when it becomes chronic. This is a simplified guide, and should not substitute real-time professional consultation. There are far more types of urticaria. But, we will condense them into these two types here, in order to cover as much as possible, with convenience.
So, let’s take this scenario;
It was a Saturday evening, you were normally living your life after you have come back from a strawberry picking trip in one of the farms. Suddenly you felt something was itching at the back of your upper arm. Curiously and instinctively you touched it, and it felt like a small bump or a few; joined together in one place, then you looked at it, and it is kind of a small pinkish-red circle. When you pressed on it, it was a little stingy.
It’s itchy again, so you scratched it, but it did not stop the itching, it actually worsened it. You decided to stop scratching and held your hands back while thinking about what to do next.
You decided that you won’t touch it again.
Immediately and thoroughly washed your hands with soap and water before even touching any other area of your body, other people, or anything else. You also washed the itchy area with some mild soap and cool water and dried it by gentle dabbing not rubbing, then you applied some Calamine lotion that you have at home to soothe it a little bit.
You waited and watched to see what happens next. After about 3 hours, it disappeared on its own without any trace. You are relieved and went to sleep peacefully 🙂
Sunday morning you had plans with the family for the day. You gathered at the beach for a mini picnic. It was a beautiful sunny day, but a little humid. You had some delicious seafood from the food truck, you had chocolate ice cream, you swam, you played with the kids, you had a blast. You are just starting your summer plans. Having a mini trip during the weekends.
At the end of the day, in the evening, you packed up heading home. On your way back, you stopped at a local park to have a nice stroll while the temperatures were cooling down.
Everything was spectacular, you are really looking for the upcoming weekend.
When you made it back home, you suddenly felt the same itchy feeling you had yesterday evening, but this time it showed up somewhere else!
On your thighs!
You looked at it, and they look like the same ones which were on your upper arm!
Ughhh!

Here is the breakdown;
A foreign particle (allergen) has entered your body and caused an antibody called IgE released to the bloodstream. The latter -with the allergen together- activated a type of cells around skin vessels called mast cells. These invite the immune system over to the area, through releasing a chemical called “histamine” -among others- mainly responsible for the itching and the manifestation of simple hives on the nearby skin surface as red, swelled up patches. These are usually seen -but not exclusively- on the extremities or the face.

What could that foreign allergen be?
You have gone to different places, ingested food, played with water under the sun, and so on.
So, answering this question could be a little bit tricky, since also, you don’t have a history of documented food or environmental allergies. You also didn’t take any medications except that Naproxen 220mg pill in the morning for your right shoulder pain, because of yesterday’s activity at the strawberry farm where you walked a long distance carrying your basket using your right arm.
Let’s agree on something here, each person’s reaction is different, but in general, hives could be triggered by allergens that come from:
Something that you inhaled
Pollen, mold spores, dust, plants or animal mites, animal dander, or even smoke (chemicals).
Something that you ate
Possibilities in your case could be seafood, chocolate, strawberry, nuts, cow milk. You never had an issue with any of these before so it might be preservatives such as azo dyes, benzoic acid derivatives, or food dyes.
Medications you take
Any medication could cause hives but not necessarily since each person is different. Alcohol is a drug and could also trigger hives.
Non-steroidal anti-inflammatory drugs like Naproxen, that you had this morning, could be one of them.
Take extra precaution when taking medications (including over the counter medications) that are photosensitizing, meaning an exposed skin to sun UV light with the presence of the medication in your body could cause eruptions, not hives, but might be other dermatological diseases.
A general recommendation is to wear a broad-spectrum sunscreen with SPF 30 or more, for all exposed skin areas, and reapply every two hours, or if the skin is wiped off, and after swimming or sweating. Choose water-resistant sunscreens. Avoid direct sun exposure if possible.
Infection(s) that you might be having
Maybe you’re having a respiratory infection and you’re not experiencing other symptoms yet, like sinus, common cold, COVID-19 :-O or other infections, like urinary tract infections.
Chemicals that you touched
Like latex, soaps, detergents .. etc
Insect bites
You went to a farm, the beach, the park, and even your back yard. Summertime is a fun time for insects as well. So, this should also be considered.
A general recommendation is to use insect repellent sprays all over your exposed areas of the body (clothes included). To choose the safe ones for pregnant or breastfeeding women, and for children. Sunscreen and insect repellents can be used safely together. Apply the sunscreen first, then the insect repellent second.
Physical factors
Exercise, heat, cold, (or temperature change), humidity, water on the skin, scratching, pinching, or stroking the skin could trigger hives.
All of the above were part of the activities you enjoyed over the past two days, so let’s keep an eye on in the future.
Your state of mind
Were you stressed, sad, or depressed?
These psychological states might also trigger hives.
Other medical conditions
Thyroid diseases, Asthma, Rheumatic diseases, and other diseases might also trigger hives.
Genetic
Having a family history of urticaria or other allergy related diseases could also be considered as a trigger.
Unknown triggers
Sometimes it is just like that, despite all efforts, the triggers stay unknown.
A little note at the end of this section here, that some of the triggers mentioned above will definitely be responsible for acute urticaria like a preservative in food for example, once you avoid it, urticaria disappears on its own. Others will trigger the chronic type especially when triggers are unavoidable or you can’t do something about it. In any case, it will start at some point, as “acute”.
What should I do right now?

- First things first, avoid the known trigger(s). If the trigger is unknown, you’ll watch for it, and try to avoid it.
- When doing outdoor activities, remember to apply sunscreen (even during winter time) and insect repellent when needed. Always keep well hydration (alcoholic beverages are not hydrating), stay in shade, wear protective clothing if possible, and avoid direct sun exposure during peak hours.
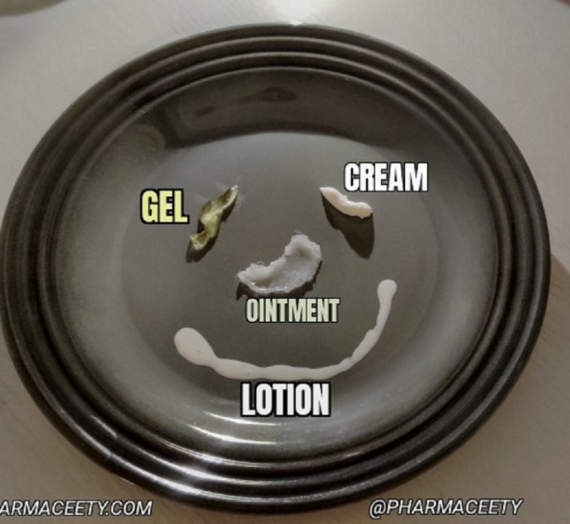
- Soothing and cooling treatments, like calamine lotion, or bathing with oatmeal-based products.
- Starting with antihistamines, medications found over the counter. The first choice would be the non-drowsy ones, These are:
Cetirizine
5 or 10 mg once daily
Desloratidine
5 mg once daily
Fexofenadine
60 mg twice a day
Loratidine
10 mg once a day
*General adult doses, children doses not addressed
- The second choice of antihistamines is the more drowsy ones. These are:
Diphenhydramine
25 – 50 mg three times or four times daily
Chlorpheniramine
4 mg four times and up to six times daily
Hydroxyzine
25 – 50 mg once daily usually at night time
*General adult doses, children doses not addressed
- There is also limited evidence to use stomach acid medications over the counter, like Ranitidine 150 mg (Zantac) and Famotidine 20 mg (Pepcid) WITH antihistamines NOT alone if the latter fail. Please consult with your healthcare provider first.
- A corticosteroid cream like Hydrocortisone 0.5% or 1% over the counter might not address hives from within, especially if the issue is greater than the affected area itself (See slides below), but it might help relieve the itching and inflammation of that spot if the area is limited. It is not generally recommended.
Other prescription options are to be discussed with your primary doctor or practitioner if all failed to control your acute or chronic hives.
Is there anything else about hives that needs to be addressed or you might be wondering about?
References, Citations and Attributions:
Kayiran MA, Akdeniz N. Diagnosis and treatment of urticaria in primary care. North Clin Istanb. 2019;6(1):93-99. Published 2019 Feb 14. doi: 10.14744/nci.2018.75010
Bettina Wedi. Urticaria and Angioedema Crossref. 2020. DOI link: https://doi.org/10.1007/978-3-662-58713-3_29-1
Stuart H Ralston. Ian D Penman. Mark WJ Strachan. Richard P Hobson. Davidson’s Principles and Practice of Medicine, 23rd Edition. Elsevier LTD. 2018
Photos credit: