Ask yourself these questions;
Do you experience frequent heartburns during the week? How many times? Less or more than 3 times a week?
If your answer is less than 3 then here is your first check mark ✔
Do you eat chocolate, spices, large fatty meals, or drink caffeinated, alcoholic, or acidic citrus beverages in excess?
If yes. Then here is your second check mark ✔
But also, do you do the above later in the day then sleep shortly after?
If yes. Then here is your, well ¿ you guessed it ☺, your third check ✔
Do you smoke?
Yes. ✔
Are you obese or pregnant? (they are not interchangeable, just bear with me ≈ )
Yes, and yes. ✔ and ✔
Now, you are heading to the pharmacy to grab a medication to help you manage these symptoms.
But, wait ⚫ I want to tell you something first …
One of the most dispensed medications I witness prescribed or chosen over the counter by patients daily is stomach acid-reducing medications.
Nowadays, they are taken chronically, comparable to other chronically given medications for high blood pressure, diabetes, and cholesterol-lowering ones.

They work wonders in the treatment of reflux acid and symptoms of heartburn, and in most cases, this is why they continue to be chosen. But, are these medications supposed to be taken for this condition chronically?
We are talking about a class of stomach acid medications called proton pump inhibitors or shortly known as PPIs.
• Lansoprazole
• Omeprazole
• Pantoprazole
• Rabeprazole
• Esomeprazole
• Dexlansoprazole
▩ In Canada, two of the above have moved from being solely prescribed into being behind/over the counter:
➛The first was Omeprazole. It is still behind the counter and you can discuss your need for it with the pharmacist.
➛The second was Esomeprazole aka Nexium, which could be found over the counter. And you could also ask the pharmacist for it.
PPIs are generally a safe group of medications. They’ve been in the market for over 30 years. Their use has increased drastically over the past decade or two. A good number of studies have followed through its side effect profile on the longer term, most were caught observationally and then a number of reviews and stronger studies followed to evaluate the many risk claims linked to this class of medications.
Let’s start by reviewing the stronger evidence then we’ll move to the weaker one.
A strong evidence supports that chronic PPIs use might cause:
☹ Low magnesium blood levels
Magnesium is one underestimated mineral in reducing muscle spasms, inflammation, blood clotting, and arrhythmias (irregular heart beats). Magnesium lower the risk of diabetes, cardiovascular and rhythmic diseases, and also prevent bone fractures. Low levels usually go undetected, but it has been found lower in chronic PPI users.
☹ Bone fractures
Maybe because of the lower magnesium levels as mentioned above. PPIs do not generally reduce Calcium absorption, except for those who take Calcium Carbonate as a source of supplementation. Absorption of other types of calcium supplements or calcium from food sources is not affected.
Bone mineral density is affected with chronic use of PPIs, generally in an unknown way. Older individuals need to pay more attention, especially older women, who could be more sensitive to bone fractures.
☹ Pneumonia
Yes, you read that right. But, how?
These medications are very strong in reducing stomach acid. Stomach acid is also important for the eradication of swallowed pathogens and bacteria (We do that every day when we drink and eat). So, when this acid is no longer enough to kill these pathogens, they’ll flourish in the digestive system, and they might colonize up to the esophagus then aspirated to the respiratory system through the trachea, into the lungs, increasing the chance of lung infections.
Do we need this with COVID-19? No.
☹ Intestinal infections such as C. Difficile
This is a nasty resistant bug, that is not affected much by stomach acid to begin with, but what is affected are other microorganisms that normally live in the gut to produce balance against the colonization of nasty ones like C. Difficile.
PPIs chronic use may alter this resistance causing increased infections of the intestine with this bacteria that may require hospitalization.
☹ Iron deficiency Anemia
In general, Iron requires stomach acid in order to be absorbed, especially the type of iron found in cereals, vegetables, and beans, which is called “non-heme” which also represents about 60% of dietary iron.
Chronic use of PPIs is linked to iron deficiency anemia.
☹ Chronic Kidney Disease
It is not well known why CKD happens with the chronic use of PPIs, but they cause acute kidney injury, this may be one of the causes that progresses into CKD (chronic kidney disease) which is irreversible.
Now, there are other claims like causing:
Vitamin B12 deficiency.Not likely, because PPIs reduce the stomach acid not enough (achlorhydria – the complete absence of acid) to cause vitamin B12 reduced absorption i.e. deficiency.
Dementiaand severe cognitive impairment: suspicions based on some observational studies. This needs more investigation and a stronger association. In the meantime, it is good to watch for any signs of cognitive deterioration if taking PPIs long term and report that to your healthcare provider.
- Cancers:
▸Colorectal cancer. There is no association between PPI use and this cancer.
▸Gastric cancer. There are some studies that confirm the association of long-term use of PPIs especially for those who also have H. Pylori infection in the stomach (a very common infection) with increasing the risk of gastric cancer (stomach cancer).
Calcium deficiency. Not likely, as mentioned before. Only one type of supplements called Calcium Carbonate requires stomach acid for better absorption. Other salts of Calcium like Citrate, or Calcium from food sources are not affected.
Some people need to stay on a PPI for a long time. However, others only need this medication for a short period of time, hence – the 14 days packages you could find over the counter.
When the ongoing reason for using a PPI is unclear, the risk of side effects may outweigh the chance of benefits.
Who needs to stay on PPIs?
Are the ones with a clear diagnosis
like:
- Barrett’s esophagus
- Long-term use of NSAIDs (nonsteroidal anti-inflammatory drugs like Advil)
- Severe inflammation of the esophagus
- Documented history of bleeding stomach ulcer
There are some other unique situations where people mistakenly end up with long term use of PPIs:
1- When patients are hospitalized for any reason, sometimes they are prescribed PPIs to prevent stress ulcers from happening. Once they are discharged from the hospital, they no longer need it. But, they continue to use it for no apparent reason.
This one is upon the pharmacist to investigate
2- Some people under ongoing stress in general, have their stress ► out ► physically
For example, for some chronically stressed, it may come out as physical muscular pain, like back pain. For others, it might involve acid reflux.
So, let’s say that you are stressed chronically
And you experience some of the worst heartburn episodes at night
It might happen daily, but after a while, it might happen occasionally only when having an acute stress episode in between (There is an increased sensitivity of the stomach lining with chronic stress).
If you are chronically stressed, you need to manage the underlying stress instead of continuing to suppress symptoms of it, like acid reflux. There is no evidence that suggests you should take the PPIs long term for this reason, rather take when needed or switching to another class as recommended by your healthcare provider. The risks are higher than the benefits if taken regularly for this situation.
3- If you are on other medications, investigate their role and effects on acid reflux with your healthcare provider. Is it possible to eliminate them?
Some examples of medications that may increase the possibility of heartburn:
- Some blood pressure medications. (Beta blockers and Calcium Channel Blockers)
- Some medications for the active bladder. (Anticholinergics)
- Some Antidepressants. (Tricyclic Antidepressants)
- Some Angina Heart medications. (Nitrates)
- Others
Now, you have learned the available and necessary information with regards to the long term use of PPIs. We have now four scenarios:
The first is, you want to do the right thing since you just started having mild symptoms of heartburn. What should you do?
Remember the few questions I asked you at the very beginning with checkmarks? ☺
The ✔answers mean you probably could manage your symptoms through:
Lifestyle changes:
• Avoid triggers (e.g. coffee, alcohol, spicy foods, chocolate)
• Avoid food 2-3 hours before bedtime
• Elevate the head of the bed
• Lose weight
If you are pregnant, then it’s normal to have a mechanical pressure of the belly on your stomach (the same way overweight does). Heartburn is normal with pregnancy, and it usually resolves after. Practice lifestyle changes mentioned above ☝ and also most over the counter medications (Avoid Gaviscon) are safe to use during pregnancy.
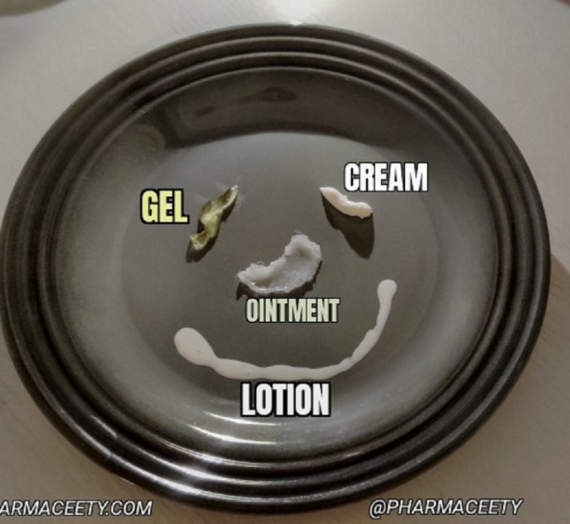
- Manage occasional heartburn with over the counter drugs, such as:
• Tums® Calcium Carbonate
• Rennie® Calcium Carbonate / Magnesium Carbonate
• Rolaids® Calcium Carbonate / Magnesium Hydroxide
• Ranitidine
• Gaviscon® Sodium Alginate / Calcium Carbonate / Sodium Bicarbonate
• Omeprazole and Esomeprazole [Reserve these PPIs for severe heartburn and only try when needed or for a maximum of 14 days – as discussed before]
The second is, you now think you’ve been using PPIs for a long time without one of the clear diagnoses discussed above (or with your healthcare provider) and you want to stop or reduce the use of these medications.
What is the best way?
It is not recommended to stop PPIs altogether if you’ve been on them for a long period of time, because of rebound acid production and reflux (80% of the time).
Should you switch to “on-demand / when needed” or slowly going down with your dosing?
Evidence from clinical practice suggests success achieved with slowly going down ✓ than switching to “on-demand/when needed” right away [Discuss that with your healthcare provider first]
Here is how to safely go down with dosing:
1- Set 4 – 6 weeks as a tapering schedule.
2- For the first week or two, start by reducing the daily dose if possible;
Reducing the daily dose might involve;
▸Taking the PPI once daily instead of twice daily
▸Lowering the number of mg (e.g. from 30mg → 15mg, or 40mg → 20mg, or 20mg →10mg, depending on the drug)
3- For the third week and on, start taking your dose every other day instead of daily before stopping.
4- During this tapering process use other over the counter medications like Zantac or Tums for breakthrough symptoms in between.
5- You could also switch to “on-demand/when needed” PPI after you safely tapered down and stopped your regular use.
What to monitor after reducing or stopping a Proton Pump Inhibitor with the help of a healthcare provider (physician, nurse practitioner, or pharmacist), it is important to check for, and report signs of:
• Heartburn
• Reflux
• Stomach pain
If heartburn, reflux, or stomach pain continues after 3-7 days and interferes with normal activities, please talk to your healthcare provider. They can help decide whether to return to a previous PPI dose or whether to use the PPI ‘on-demand’ (daily until your symptoms stop). They may also suggest a test for a treatable condition called H. pylori.
The third is, you have a heartburn but you also:
• Can’t eat / Lost appetite
• Unintentionally lost weight
• Difficulty/Pain when swallowing food
• Dark stool
Report these signs to your healthcare provider. These might need further investigation, do not just self treat.
The fourth is, you determined after consulting with your healthcare provider, and you have one of the clear diagnoses mentioned earlier, that a need for PPIs long term (more than a month).
What should you watch for?
- Watch for upper respiratory tract infections. Get the necessary vaccinations like pneumonia vaccine and the flu vaccine, (and soon, COVID-19). If you use inhalers to control symptoms of Asthma or COPD, keep using them properly to prevent worsening of your symptoms. Keep good hand hygiene, and stay away from sick and non-sick people alike, and wear your mask (We are still in a COVID-19 pandemic ♾).
- Watch for any signs of anemia, check with your doctor if you feel fatigued or having a foggy brain, check your iron levels. And if you are older check your Vit B12 levels as well.
- Keep your magnesium at normal levels. Long term use of PPIs will prevent normal absorption of magnesium from the diet, so use magnesium supplements like magnesium citrate or magnesium chloride.
- You could also use Calcium supplements like calcium citrate (not calcium carbonate) if you have low calcium levels. Keep your vitamin D at normal levels as well.
- Watch for any cognitive deterioration, and report that to your healthcare provider.
- Watch for increased episodes of sudden diarrhea and report to your healthcare provider.
- Manage stress. Incorporate exercise to do so.
- With the help of your doctor, monitor your kidney function, especially if you are older.
- Consider periodic reassessment of your need to continue your PPI intake, and discuss reducing the use/stopping them with your healthcare provider.
One last stressing note before I wrap up this article.
Bear in mind that it is:
✴About proper use (meaning that you should have one of the clear diagnoses) over improper use.
✴And about short term use as much as necessary possible, over long term use (problems happen with the long term use).
These are the pearls ☝
If you have any other questions or something else that I need to highlight, please comment below.
Thank you ☺
References, Citations and Attributions:
1.Barbara Farrell, Kevin Pottie, Wade Thompson, Taline Boghossian, Lisa Pizzola, Farah Joy Rashid, Carlos Rojas Fernandez, Kate Walsh, Vivian Welch, Paul Moayyedi. Deprescribing proton pump inhibitors, Evidence-based clinical practice guidelines. Canadian Family Physician May 2017, 63 (5) 354-364;
2. Megan Jaynes, Avinash B. Kumar. The risks of long-term use of proton pump inhibitors: a critical review. Sage Journals. November 19, 2018 Review Article https://doi.org/10.1177/2042098618809927
3. Daniel E. Freedberg. Lawernce S. Kim. Yu-Xiao Yang. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. AGA. Volume 152, Issue 4, P706-715, MARCH 01, 2017 DOI: https://doi.org/10.1053/j.gastro.2017.01.031
4. Jan Zirk-Sadowski, Jane A. Masoli, Joao Delgado, Willie Hamilton, W. David Strain, William Henley, David Melzer, Alessandro Ble. Proton‐Pump Inhibitors and Long‐Term Risk of Community‐Acquired Pneumonia in Older Adults. The Journal of the American Geriatrics Society. 20 April 2018 https://doi.org/10.1111/jgs.15385
5. Avinash K. Nehra, Jeffrey A. Alexander, Conor G. Loftus, Vandana Nehra. Proton Pump Inhibitors: Review of Emerging Concerns, Mayo Clinic Proceedings, Volume 93, Issue 2, 2018,Pages 240-246,ISSN 0025-6196. https://doi.org/10.1016/j.mayocp.2017.10.022
6. Sean A.P. Clouston, Oren Shapira, Roman Kotov, Lan Lei, Monika Waszczuk, Evelyn J. Bromet, Benjamin J. Luft. Proton pump inhibitors and the risk of severe cognitive impairment: The role of posttraumatic stress disorder,
Alzheimer’s & Dementia: Translational Research & Clinical Interventions.
Volume 3, Issue 4, 2017, Pages 579-583, ISSN 2352-8737. https://doi.org/10.1016/j.trci.2017.08.007.
7. Yan Xie, Benjamin Bowe, Tingting Li, Hong Xian, Yan Yan, Ziyad Al-Aly, Long-term kidney outcomes among users of proton pump inhibitors without intervening acute kidney injury, Kidney International, Volume 91, Issue 6, 2017, Pages 1482-1494, ISSN 0085-2538. https://doi.org/10.1016/j.kint.2016.12.021
8. Cho, Yu Kyung. “Can Acute Stress Cause Esophageal Hypersensitivity in Healthy Individuals?.” Journal of neurogastroenterology and motility vol. 23,4 (2017): 483-484. doi:10.5056/jnm17118
9. Michael Boxer. Iron deficiency anemia from iron malabsorption caused by proton pump inhibitors. 01 September 2020 https://doi.org/10.1002/jha2.96
10. Tran‐Duy, A, Connell, NJ, Vanmolkot, FH, Souverein, PC, de Wit, NJ, Stehouwer, CDA, Hoes, AW, de Vries, F, de Boer, A (Maastricht University Medical Center, Maastricht, the Netherlands; University of Melbourne, Melbourne, Australia; Maastricht University, Maastricht; Utrecht University; University Medical Center Utrecht, Utrecht, the Netherlands). Use of proton pump inhibitors and risk of iron deficiency: a population‐based case–control study. J Intern Med 2019; 285: 205– 214.
11. Ka Shing Cheung, Esther W Chan, Angel Y S Wong, Lijia Chen, Ian C K Wong, Wai Keung Leung. Long-term proton pump inhibitors and risk of gastric cancer development after treatment for Helicobacter pylori: a population-based study. 2018;67:28–35. doi:10.1136/gutjnl-2017-314605
13. Ito, Tetsuhide, and Robert T Jensen. “Association of long-term proton pump inhibitor therapy with bone fractures and effects on absorption of calcium, vitamin B12, iron, and magnesium.” Current gastroenterology reports vol. 12,6 (2010): 448-57. doi:10.1007/s11894-010-0141-0
14. Fohl, Alexander L, and Randolph E Regal. “Proton pump inhibitor-associated pneumonia: Not a breath of fresh air after all?.” World journal of gastrointestinal pharmacology and therapeutics vol. 2,3 (2011): 17-26. doi:10.4292/wjgpt.v2.i3.17
15. Kuiper, JG, van Herk‐Sukel, MPP, Lemmens, VEPP, Kuipers, EJ, Herings, RMC. Proton pump inhibitors are not associated with an increased risk of colorectal cancer. GastroHep. 2020; 2: 165– 170. https://doi.org/10.1002/ygh2.409
16. Help patients take the first OTC PPI appropriately. The pharmacist letter Canada. February 2019
17. Help put the risk of Dementia with PPIs in perspective. The pharmacist letter Canada. April 2016